Faecal Bile Acids
Bile acids are included in the GI EcologiX host health markers section.
The all-important GI health marker section provides a comprehensive analysis of:
Immunology & inflammation – SIgA, calprotectin, Beta defensin 2
Digestion – pancreatic elastase 1, bile acids
Mucosal barrier integrity – zonulin
Tissue abnormalities – FIT (occult blood)
What are bile acids?
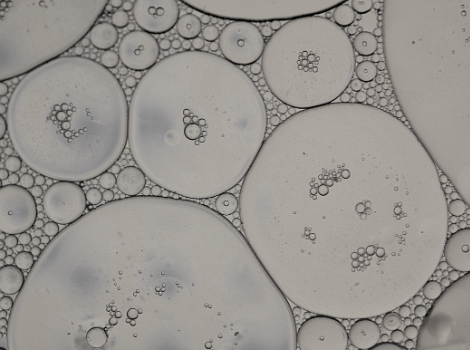
Bile acids are steroid molecules that emulsify fat, facilitating its digestion and absorption, along with fat-soluble vitamins (A, D, E and K). Once bile acids have fulfilled their function, they are reabsorbed and brought back to the liver where they regulate the synthesis of cholesterol. Bile acids are also an important component of our eliminatory system, getting rid of waste products via bile in the faeces.
The gut connection
Most bile acids are reabsorbed in the small intestine with only a small amount reaching the large intestine. Here they are metabolised by gut bacteria into secondary bile acids, which have important signalling properties, regulating host metabolism as well as playing a role in the onset of metabolic diseases such as Type 2 diabetes mellitus (T2DM), cardiovascular disease (CVD) and non-alcoholic fatty liver disease (NAFLD). Disrupted bile acid metabolism related to a dysbiotic gut microbiota has also been associated with the development of IBD and cancer. In the small intestine, low bile acids may enable, or be a causal factor, in SIBO.
What do the results tell me?
Low bile acids
Bile acids have antimicrobial properties, so low bile acids may enable a dysbiotic microbiota in the small (SIBO) and large intestine. Because bile acids are crucial for eliminating waste, low bile acids can impact the breakdown of metabolic waste, which can cause constipation and flatulence.
Bile salts when they reach the ileum bind to a receptor known as the farnesoid X receptor (FXR). FXR is responsible for some of the negative feedback system of recycling bile salts, but equally it is responsible for stimulating the release of antimicrobial peptides in the ileum. This means low levels of bile salts might be associated with poor mucosal immunity of the intestine.
Bile salts are also an important regulator of small and large intestine movements via the migrating motor complex, so a lack of bile acids may result in constipation, or be a contributing factor towards SIBO, which in turn can lead to diarrhoea.
High bile acids
When bile acid excretion levels are higher than expected, it may be linked to symptoms of osmotic diarrhoea, or symptoms that are often labelled as irritable bowel syndrome (IBS).
High levels of secondary bile salts can cause inflammation, oxidation and damage to the epithelial lining of the intestine, and high levels may impact other feedback loops such as detoxification processes in the liver, and it may upregulate endogenous cholesterol production.
Reduced resorption of bile acids (which will show as elevated on a stool result) may be due to damage to the small intestine due to inflammatory bowel disease, cancer intervention, coeliac disease, bowel resection, dysbiosis (especially of bacteria that can deconjugate bile salts such as Clostridium perfringens, Bilophila wadsworthia, Desulfovibrio spp.), SIBO, gall bladder removal or for other unknown reasons.
High bile salts can also lead to inflammation and damage to the epithelial barrier, increasing the risk of colon cancer.
What dietary interventions can we make?
Low bile acids
The use of choleretic and cholagogue herbs, such as globe artichoke, milk thistle, dandelion and burdock may help to regulate bile production, flow, secretion and resorption. Digestive support with pancreatic enzymes such as lipase, exogenous bile acids and hydrochloric acid may also be helpful.
High bile acids
Increasing the amount of fibre in your diet, especially pectin, cellulose, and specialised fibres such as partially hydrolysed guar gum (PHGG) can help to bind excess bile salts and excrete them to prevent irritation at the gut wall. Reducing the amount of fats in your diet, especially saturated and trans fats, can help to reduce symptoms. In cases of bile acid diarrhoea, a very low-fat diet of under 40g a day is recommended to help to control extreme symptoms, as well as reducing the amount of refined sugar in the diet. Additionally, small, regular meals may help to prevent a large output of bile from the liver.
Bile acids are conjugated with taurine or glycine before being secreted and utilised in the intestine. Adding sources of taurine and/or glycine-rich protein with fatty meals may reduce symptoms.
The use of bitter herbs such as choleretics and cholagogues, may help to increase both the production and flow of bile, and also support the healthy resorption of bile.
Underlying causes such as dysbiosis and/or SIBO should be looked into with the help of a healthcare professional.
Please see our GI Clinical Considerations and Interpretive Guide (logged in only) in the resource section for more information.