What is the Oral Microbiome and why should you take care of it?
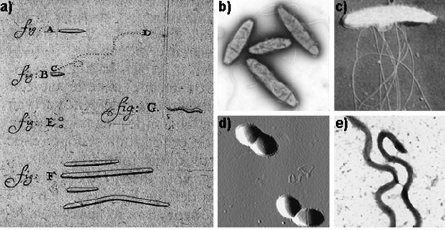
In 1683, Antonie van Leeuwenhoek, affectionately known as the ‘Father of Microbiology’, paved the way for the first research into the human microbiome. In a letter sent to the Royal Society of London, he described and illustrated five different types of bacteria that he was able to distinguish from his mouth using a handcrafted microscope1. Van Leeuwenhoek decided not to clean his teeth for three days so he could collect the “material that had lodged in small amounts on the gums”. He then sketched these microbes in his notebook, unknowingly being the first to ever draw dental plaque and the most abundant bacteria in the oral cavity: Streptococcus mutans. Fast forward 200 years and we have now discovered that the oral cavity has the second largest and most diverse microbiota after the gut. It harbours over 700 different species of bacteria as well as being home to approximately two billion bacteria2. Whilst the oral microbiome is one of the most well-studied microbiomes due to ease of data collection, unfortunately, it has never received the spotlight and attention it deserves. Unlike its relatives the gut, skin, and vaginal microbiomes, the oral microbiome has remained in the shadows, rarely mentioned. Between 2013 and 2017, the number of publications focused on the gut microbiome made up to 80% of the total publications on the microbiome over the last 40 years3. Furthermore, the global probiotics market aimed at gut and urogenital health is projected to reach $77.09 billion by 2025 according to a report by Grand View Research, with an increase of 7.7% in 20194. Probiotics aimed at the oral microbiome were unfortunately excluded from the ‘probiotic market’ and research into support of the oral microbiome is lagging compared to research performed on other microbiomes.
The oral cavity has the second largest and most diverse microbiota after the gut. It harbours over 700 different species of bacteria as well as being home to approximately two billion bacteria.
The mouth is a unique part of the body. Unlike other microbiomes, the oral microbiome is highly heterogenous, meaning it supports the growth of numerous different microbial communities all under the same ‘roof’. The teeth, cheeks, gums, tonsils, and the hard and soft palates provide different environments for microorganisms within the same mouth. Furthermore, the oral cavity provides the ideal environment for the growth of microorganisms. It is warm, moist, and highly nutritious. The saliva of the mouth provides the perfect medium for transportation of nutrients. Think of it as an all-you-can-eat buffet for microorganisms (including free delivery!). The saliva not only delivers nutrients but is also rich in enzymes and proteins that are able to neutralize the pH of the mouth and fight away unwanted bacteria. Saliva is your mouth’s best friend and is integral in maintaining balance and equilibrium2. The teeth are the only natural non-shedding surface in the human body, which allows for extensive biofilm formation and maturation5. That means if you do not brush your teeth (like Van Leeuwenhoek), certain bacteria can colonize and mature. To make matters even more difficult, we dentists add more non-shedding surfaces in the mouth such as dental restorations, crowns, implants, and dentures. This can further influence biofilm formation and composition. Due to the high variability of the oral microbiome, its numerous ecological niches, and its proximity and constant exposure to external forces, the oral microbiome is a tough nut to crack. Every time you breathe, eat, drink, smoke, take medication or forget to brush your teeth, you put the delicate balance of the oral microbiome at risk.
So what happened to the oral microbiome?
To my dismay, the oral microbiome hasn’t quite got the publicity I believe it deserves. Whilst the public understands the importance of gut, skin, and urogenital health, many turn a blind eye to oral health and don’t even know their mouth has a microbiome. Whilst you may take probiotics, prebiotics and change your diet to optimize gut health, very few would do the same to optimize their oral health. If you one day woke up flatulent or bloated, you would be concerned and seek professional help. Gastrointestinal discomfort directly impacts your day, the way you feel, and even the way you look. However, many people are not concerned when they find their gums bleeding when they brush their teeth. In fact, only three percent of Americans seek professional advice and support for gum disease6, even though 50% of the American population suffers from bleeding gums. Our mouths are hugely forgiving, and we often take this for granted. Signs and symptoms from the mouth will only become noticeable to a person (and even most dentists) when oral microbiome dysbiosis is very severe and irreversible damage has occurred. Unlike the gut, where flatulence or bloating may be warning signs of the beginning of dysbiosis, the mouth, unfortunately, gives very few visible and noticeable warning signs.
The connection between dental plaque and oral diseases was long established by G.V Black in 1898, where he discovered that the cause of dental caries was due to the attack from acids generated by bacteria within these plaques7. This inspired much scientific investigation into plaque. There has been, however, a lack of suitable cultivation techniques and gaps in knowledge of the oral microbial flora until relatively recently. Scientists and dentists were under the assumption that oral diseases such as gum disease and decay were caused by a physical increase in bacteria and plaque, not due to qualitative differences in the composition of the bacteria7. As a result, instead of treating decay or gum disease as an infectious disease, traditional dentistry is primarily focused on removing the mass of dental plaque. Whilst mechanical removal of plaque is of course needed (hygiene appointments are very necessary), if one’s microbiome is altered or pathogenic, removing all the bacteria (including good bacteria) during a clean is not enough. One should remove the bacteria and create an environment for a healthy microbiome to prosper. Otherwise, the same unhealthy bacteria will continue to dominate and cause problems. This can only be done by understanding what bacteria is present at that time in the mouth and tailoring support to restore balance. Dentists do not often attempt to understand the unique microbiome of their clients, let alone attempt to modify it to make it less pathogenic. Instead, they often treat the damage once it has been caused (such as filling a cavity), rather than preventing damage from occurring in the first place.
Dentists and clients would benefit from using plaque and saliva samples for early detection and quantification of the bacteria known to cause gum disease and decay. This would help clinicians take preventative measures to stop oral microbiome dysbiosis and therefore reduce the risk of developing gum disease, decay, and other oral diseases. To put this into perspective, compare it to the early detection of cancer markers in the blood before cancerous lesions develop7. In all other fields of medicine, biomarkers and analysis of bacteria are used to predict disease risk. If you are concerned that you may be pre-diabetic, you would check your glucose levels to assess your risk of developing diabetes. If you were concerned you were overweight, you would weigh yourself using a scale. Why shouldn’t Dentistry be the same?
Furthermore, it is not just the quantity and quality of the microbiome that will dictate whether a clients has disease, but also how the body responds to an altered microbiome8. With our new understanding of the oral microbiome and its interactions, the use of probiotics for the oral cavity has become more popular. More evidence is showing that probiotic therapy could be used to maintain oral health, reduce the risk of decay, and reduce the risk of periodontal disease9,10, though more research is needed.
The mouth is not only the mirror of the body but also the gateway.
Why is the oral microbiome so important?
The mouth is not only the mirror of the body but also the gateway. Many argue that the oral microbiome is an extension of the gut and with that logic, deserves as much attention. Many gastrointestinal diseases such as Ulcerative Colitis or Coeliac Disease appear first in the mouth before symptoms occur in the gut. This is because the mouth has a fantastic blood and nerve supply, with a more rapid cell turnover than any other part of the body.
Growing research has shown that oral health not only prevents oral issues like decay, gum disease, and bad breath but also has positive effects on the rest of the body. When the microbiome is imbalanced and disease occurs, high levels of pathogenic bacteria and its associated chronic low-grade inflammation can have catastrophic effects on the body. Clients with gum disease are three times more likely to suffer from Diabetes Mellitus11, three times more likely to be obese12, three times more likely to suffer from heart disease13 and 70% more likely to develop Alzheimer’s Disease14.
It is time to start thinking that a healthy body includes a healthy mouth.
Top tips to maintain a healthy oral microbiome
- Visit your dentist regularly (if you can) to ensure that you have a healthy mouth. Don’t go only when you have issues. Make it a regular trip!
- Have a professional clean regularly. Recall intervals vary depending on your hygiene. Ask your hygienist/dentist what they think is best.
- Get Guided Biofilm Therapy (GBT). This is a procedure that replaces the old fashioned scale and polish. The advantage of GBT is that it is a systematic, predictable, and elegant solution for dental biofilm management in prophylaxis of dental decay, gum disease, and oral microbiome dysbiosis.
- Test your Oral Microbiome! Find out what bacteria are present with an annual in-depth oral microbiome test. The Oral EcologiX oral microbiome profile tests for oral bacteria that can lead to gingivitis and caries, as well as systemic conditions like cardiovascular disease. Your oral health is key to whole-body health, so use this preventative tool and be proactive with your health!
- Brush your teeth twice a day for two minutes with a highly mineralising toothpaste. Try to not rinse your mouth with water after brushing and only spit out the residual toothpaste left following brushing. This way you keep all the good stuff on your teeth.
- Use Sodium Lauryl Sulphate (SLS) free toothpaste. SLS is a harsh foaming agent known to be destructive to the oral microbiome and the cells that line your mouth.
- Clean between your teeth either with floss or interdental brushes. Nearly 30% of plaque and bacteria are found between the teeth.
- Swap your mouthwash for Bio.Me Oral probiotic mouthwash. Most mouthwashes contain alcohol which can aggravate the microbiome and strip away the good bacteria. Bio.Me Oral is a refreshing probiotic mouthwash that contains strains that help establish a healthy oral microbiome and compete with oral pathogens. Your teeth feel so clean after too! Use up to twice daily between meals to freshen up and help remove plaque from the teeth.
- Nutrition is vital to maintaining a balanced microbiome. Try to eat mineral-rich foods that are alkalizing, anti-inflammatory and high in antioxidants. Mushrooms for example contain natural compounds like erythritol, adenosine, and copalic acid – compounds that are anti-microbial and antioxidant. Remember to also keep hydrated! Often bad breath can originate from dehydration.
- Scrape your tongue! What originally started as an Ayuverdic self-care ritual has now evolved into a scientifically accepted way of removing bacteria, food debris, fungi, toxins, and dead cells from the surface of the tongue. It also has proven to balance the oral microbiome and reduce the risk of systemic diseases as well as decay and gum disease. There is the added benefit of improved taste and improvement in bad breath too!




