The markers on the GI EcologiX gut health and microbiome profile were chosen because of the wealth of research and human clinical data on their relation to chronic disease. We see patterns of disturbance in certain conditions, and in this article, we will walk you through patterns of host (human) markers and microbial imbalance associated with Inflammatory Bowel Disease (IBD) and Irritable Bowel Syndrome (IBS).
Host Markers
Calprotectin
Calprotectin is a protein produced by neutrophils and is detected in the stool when there is migration to the epithelial lining due to damage and inflammation of the mucosal layer of the intestine.
Calprotectin has a distinct reference range, where anything over 100ug/g is classed as ‘high’. The NHS, prompted by NICE guidelines, classifies levels of 100ug/g and above as a trigger for a second test to investigate if the inflammation was transitory, or something that needs further investigation to rule out possible IBD. Levels of over 250ug/g are sent directly to investigation.
Mid-range levels of inflammation (between 50ug/g-175ug/g) is typically associated with IBS. Levels in acute IBD are normally seen well into the hundreds.
Calprotectin is a screening marker. If there has been one high reading, we always recommend taking a second reading four to six weeks after, as levels do change often. If there are two consistent high readings, then further investigation should be arranged.
Human Beta Defensin 2
Human beta defensins are inducible anti-microbial peptides that are associated with our innate host defence. They are induced by microbes and may play a role in our adaptive immune responses by recruiting dendritic and T cells to the site of microbial invasion. Human beta defensin-2 (HBD-2) has been shown to elevate to numbers over 100ng/g in ulcerative colitis (IBD) patients, and around 75ng/g in IBS patients, whereas healthy controls stay under 30ng/g1.
Normative levels of HBD-2
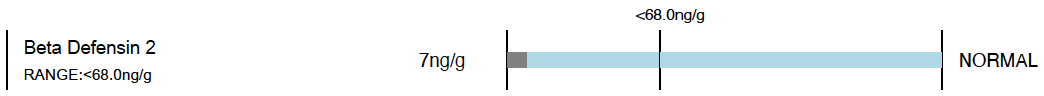
High levels of HBD-2 – have IBD in mind when looking at other markers
Microbial Markers
Commensal Bacteria – Missing Diversity + Overabundance
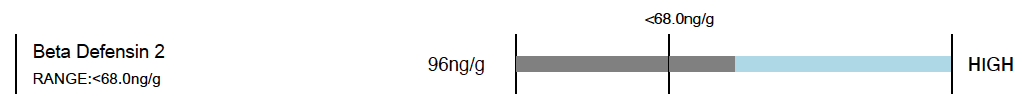
In patterns of IBD, one of the outstanding things that can show up is a lack of diversity of commensal bacteria – especially the short chain fatty acid (SCFA) producing bacteria. SCFA are important fuel sources for the enterocytes – our gut cells – so are necessary in times of mucosal tissue repair. In patterns of IBD these microbes are often found to be there in very small abundance, or not there at all. Coprococcus, Roseburia, Faecalibacterium, and Ruminococcus have all shown to be lowered in cases of Crohn’s disease (IBD), whilst in ulcerative colitis the abundance of Bacteroides, Enterococcus, Blautia, and Escherichia-Shigella have been shown to increase. The importance here is not to focus on single species, but to focus on the abundance in relation to the diversity of microbes.
This reduced diversity may also show within the Bacteriodes sub-group as missing species, or sometimes with the presence of the enterotoxigenic form of Bacteriodes fragilis. Here again, diversity is key, because an imbalance within this group can allow more inflammatory and mucin-degrading behaviours to proliferate when not kept in check by the other members of the group.
This is an example of an unhealthy diversity of the Bacteriodes sub-group. You can see the presence of the enterotoxigenic form of B. fragilis, which can be a trigger for inflammation. You can also see the three species missing, which leaves B. fragilis and B. vulgatus unopposed, allowing them to take on a more pro-inflammatory archetype.
Pathogens & Pathobionts
Our commensal microbes possess the ability to turn pathogenic in the right environment and circumstance, this is termed ‘pathobiont’. Some pathobionts, when present in higher abundance than we expect and coupled with low diversity of other species, often play triggering or mediating roles in IBD.
Fusobacterium nucleatum, an oral commensal, has been associated with colorectal cancer (CRC), inflammatory bowel disease (IBD) and appendicitis2.
Clostridium difficile and its associated toxins have been associated with mucosal colitis and colorectal cancer3.
Malassezia restricta is a fungi that has been associated with Crohn’s disease4.
Bacteroides fragilis (enterotoxigenic) has also been associated as a trigger for IBD5.
Often in cases of IBD we also see flourishes of growth of other Gram-negative bacteria, creating a high lipopolysaccharide (LPS) load, which in itself significantly increases immune responses and inflammation.
Mucin-Degradation in IBD
Damage to the mucosal lining is very much associated with IBD patterns. We can often see this reflected in the bacteria in a pattern of missing, or lower than the detectable limit (<DL) Akkermansia muciniphila, species within the Bacteriodes sub-group, and increased Ruminococcus gnavus and Ruminococcus torques, possibly combined with a raising Zonulin family peptide. Even in a healthy individual, Akkermansia muciniphila takes up little ‘real estate’ and is also good at hiding within the mucosa, so we typically see it in the low abundance ratings.
Patterns in IBS
Microbial patterns in IBS can vary greatly, as there are so many different ‘forms’ of IBS; it often is a perfect storm of factors for each individual. Contributing factors to look for are low digestive function, small intestine bacterial overgrowth (SIBO), overgrowth of gas-producing bacteria (such as the hydrogen sulphide gas-producing Desulfovibrio, or the methane gas producer Methanobrevibacter smiithi, general dysbiosis and low diversity, presence of pathogens and also other factors such as the impact of stress on GIT function.
In Conclusion
In cases of IBD, we expect to see mucosal degradation, overt inflammation, absence of commensal diversity and increased abundance of pathobionts. With this information in mind, we can choose a dietary, prebiotic, probiotic and mucosal support intervention tailored to the needs of the individual.
If you have any questions, please get in touch with us. For other GI EcologiX related education, please head here and also check your clinical resources in your account dashboard.