Imagine this common clinical presentation. A client with chronic digestive issues, ranging from constipation to abdominal discomfort and diarrhoea, and systemic health issues such as atopy and autoimmunity, has a private comprehensive stool test conducted after a conventional investigation has been unable to identify the underlying causes of their signs and symptoms.
Private stool testing can be informative in this scenario through its ability to investigate a wide range of actionable gastrointestinal tract (GIT) imbalances which might be driving this collection of symptoms. One of the most widely recognised GIT drivers of this clinical presentation is intestinal dysbiosis characterised by an overgrowth of pathogens (disease-causing microbes) and/or pathobionts (commensals which can become pathogenic under specific circumstances), including parasites (e.g. Dientamoeba fragilis), Clostridium difficile, and Enterotoxigenic Bacteroides fragilis (ETBF).(1) However, we often analyse stool test reports with no overt signs of such microbial overgrowth, either from the host markers or microbiome analysis, but the client is clearly struggling with a plethora of symptoms.
When we scrutinise such a stool test report for other possible drivers, we often detect a pattern of missing commensal (resident) bacteria, so-called ‘missing microbes’.(2) In other words, what is not present rather than what is. The purpose of this article is to shine a light on the clinical significance of otherwise hidden stool test patterns of missing microbes in the gut, how these can insidiously drive a client’s currently unexplained health issues, and what we can do to nurture the commensal gut microbiome to help restore balance to the intestinal ecosystem and improve overall health outcomes.
Missing Microbes
Dr. Martin Blaser, physician and microbiologist, coined the term ‘missing microbes’ as the title of his important 2014 book which sounded an alarm about the profound negative impact of antibiotic over-use on the gut microbiota and human ecology, and how marked disruption of the commensal gut microbiota can go on to drive disease.(2) This includes inflammatory bowel disease (IBD), obesity, asthma, irritable bowel syndrome (IBS), depression, and potentially loneliness too. (2–7) Beyond antibiotics, such disruption is driven by a wide range of other environmental as well as host factors, such as the standard Westernised diet (e.g. low fibre, high fat, high refined carbohydrates), high alcohol intake, and excessive exercise and emotional stress.(8) Nowadays, all of us are exposed to some, if not all, of these factors to some degree, a situation which has never been seen before in human communities until the last couple hundred years of modernisation.
Commensal Bacteria and the Intestinal Ecosystem
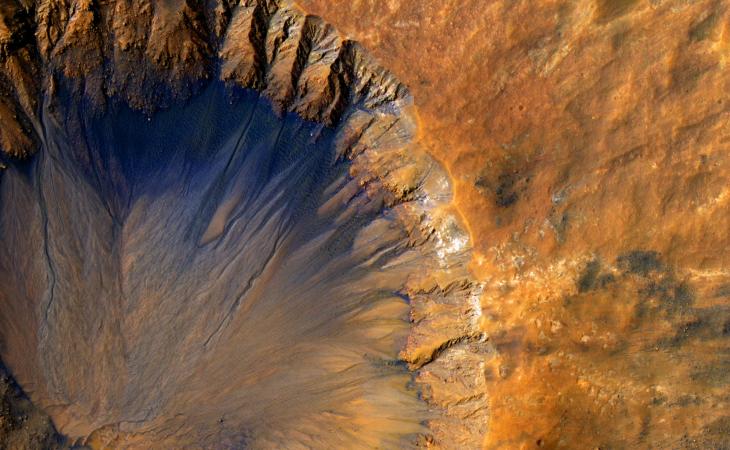
“Imagine a virgin rainforest, verdant and dense with life: insects rule the undergrowth and primates hoot from the canopy. Now see the loggers move in, chainsawing the forest’s leafy infrastructure, established over millennia, and bulldozing the rest. Imagine too a weed invading, perhaps having hitchhiked as a seed on the wheels of the diggers, and then crowding out the natives as it takes hold. The forest will regrow, given time, but it will not be the same pristine, complex, unspoilt habitat it was before. Diversity will drop. Sensitive species will die out. Invaders will flourish” Allana Collen (9)
This brief tale of a virgin rainforest echoes the natural order of the human gut microbiota and the fundamental importance of species diversity. It is now well-recognised that the more diverse the species composition of the gut microbiota, the better.(5,10) Such diversity has a multitude of downstream local and systemic health benefits, much of which stems from a phenomenon called bacterial syntrophy.
When any big, complex task needs to be completed in our daily working life, it is generally always best for several team members to be involved, co-operating, and complementing each other, with each focusing on a smaller task which meets their specialism, to help the team efficiently complete the overall task with little collateral damage. The same is true for the gut microbiota. The gut microbiota is instrumental in the simultaneous completion of a staggering array of tasks, ranging from supporting the mechanics of digestion to regulating the gut barrier, priming the immune system, and communicating with the brain via the gut-brain axis.(11) The word ‘syntrophy’ has been coined to describe this cooperation between organisms.(12)
Bacterial syntrophy is where two or more microorganisms depend on each other to fulfil their nutritional requirements, metabolism, and survival. One microorganism metabolises a specific substrate (e.g. fibre) into a chemical compound (e.g. a short-chain fatty acid – SCFA) which is required by another microorganism living within the same ecological niche. The initial ‘caregiver’ microorganism will receive a ‘reward’ in return in the form of another type of chemical compound which it needs for the same reasons. This mutually beneficial nutrient exchange is also known as ‘cross-feeding’. The net effect of this syntrophic interaction is that the whole ecosystem gets fed and every organism living within it (e.g. in the human gut microbiota) and associated with it (e.g. us, the host) experiences good health.(12)
A great example of a syntrophic relationship is that which occurs between Bifidobacterium spp. and Faecalibacterium prausnitzii. Prebiotic inulin-type fructans (a type of fibre) feed the growth of Bifidobacterium spp. Acetate, a type of SCFA, is produced as an output of this metabolic process, which can then be utilised by F. prausnitzii. One of the main outputs of F. prausnitzii metabolism is the all-important butyrate, another type of SCFA. (13,14) Butyrate is required to maintain a healthy gut barrier and has systemic benefits too, not least for modulating inflammation and supporting metabolic health.(15) Thousands of other syntrophic relationships exist between the many species which should comprise a healthy human gut microbiota, including the Bacteroides genus,(16) and the health benefits for both microbe and host are profound. Maintenance of a diverse human gut microbiota collectively helps to:
- Maintain a healthy mucosal and epithelial barrier. Akkermansia muciniphila helps to regulate mucin production and Bacteroides helps to stimulate secretory IgA (sIgA) production, which collectively supports the structure and function of the mucosal barrier.(17–19) Meanwhile, the Bifidobacterium spp./F. prausnitzii syntrophic relationship increases the production of butyrate which is required to help maintain the gut epithelial barrier.(13)
- Stave off the overgrowth of pathogens and pathobionts, partly through space occupation which helps to ‘crowd out’ these species which, in turn, helps the gut to become more resilient to infection. This is akin to how species-rich ecosystems are generally less susceptible to pathogenic invasion and disease.(20,21)
- Support normal bowel motility, partly through the ability of commensal bacteria to stimulate electrical activity in smooth muscle cells in the GIT. (22)(23)
- Support digestion and absorption. For example, Lactobacillus metabolise lactose into lactic acid.
Of course, this is only a snapshot of the importance of the gut microbiota for maintaining a healthy GIT and each of the above modes of action supports systemic health, including a strong, balanced immune system, inflammation resolution, and metabolism.(11) It is worth noting that Lactobacilli colonies living in other human microbiome sites, notably the vagina, have a similarly important role in maintaining homeostasis.(24)
When we think back to the virgin rainforest analogy, it becomes crystal clear that our gut microbiota should be able to regulate itself when given the conditions that it needs to thrive, principally ample and diverse fibre intake to foster bacterial syntrophy and as little exposure as possible to stressors such as antibiotics. This is the exception rather than the rule in our modern world and the downstream negative impact of the resultant missing microbe picture on human ecology and health can be far-reaching.
The Impact of Missing Microbes on Health Outcomes
When colonies of important SCFA-producing commensals start to diminish, the commensal species which rely on these ‘missing microbes’ for their own metabolism may diminish too or start to seek alternative sources of fuel. When the Bacteroides sub-group, for example, develops poor species diversity when fibre intake is low, Bacteroides thetaiotaomicron can switch to feeding off the mucin in our mucosal barrier instead. This, in turn, drives degradation of the mucus layer which is associated with negative health outcomes, including reduced resilience to GIT infection, inflammation of the gut wall, and IBD (25). Crohn’s, a type of IBD, is often associated with reduced abundance of Bacteroides spp., as well as several other commensals including Roseburia spp. and F. prausnitzii (26). Gut mucosal and epithelial barrier dysfunction may be exacerbated if Akkermansia muciniphila, as well as F. prausnitzii for example, become less abundant too.(29,30) When other keystone species such as Lactobacillus spp. and/or Bifidobacterium spp. drop in abundance, individuals can start to experience dysregulated bowel motility, especially chronic constipation/IBS-C. (31)
Missing microbes create the ideal environment for pathogens and pathobionts to proliferate, increasing the likelihood of GIT infections and disease. For instance, intestinal growth of the Gram-negative bacteria Fusobacterium nucleatum, an oral commensal, has been associated with IBD and colorectal cancer (CRC).(27) It can also increase the pathogenicity of commensals, as in the case of E. coli which may have the opportunity to become an issue when Bifidobacterium spp. colonies are diminished.(28)
Overall, low gut commensal diversity can drive reduced SCFA production, overgrowth of pro-inflammatory microbes, mucin degradation, intestinal hyperpermeability, and metabolic endotoxaemia (circulation of bacteria-derived toxins into circulation which can drive systemic inflammation).(32) This can then drive local as well as systemic health issues as already touched upon throughout. For example, diminished colonies of Bifidobacterium adolescentis is associated with asthma, and Akkermansia spp., Bifidobacterium spp. and F. prausnitzii with metabolic syndrome.(4,33–35)
Missing Microbe Stool Test Patterns
Commensal Bacteria
- A good indicator of diversity within the commensal gut microbiota is the presence of all key SCFA-producing commensal bacteria, with a high or very high abundance of Bacteroides, F. prausnitzii, and Ruminococcus bromii for those living in a Westernised country with food abundance.
- If some of these species are under the detectable limit (<DL), or have very low or low abundance, this is an initial warning sign of a missing microbe picture.
- Looking further to which microbes are <DL or trending in that direction reveals more patterns. For instance, ‘missing’ Akkermansia muciniphila highlights the need to assess the presence of other markers (host or bacterial) which may indicate mucosal barrier issues, such as increased abundance of the mucin-degraders, Ruminococcus gnavus and -torques.(36) Meanwhile, reduced abundance of Lactobacillus and Bifidobacterium spp., and a low ratio of Bifidobacterium to E. coli, can help us to further understand underlying drivers of chronic constipation and inflammation respectively.
Bacteroides Sub-Group
Bacteroides spp. usually takes up a lot of space within the human gut microbiota, so by assessing the composition of this genus in depth, we deepen our understanding of the balance of the commensal gut microbiota:
- Within this sub-group, we expect each of the species to be present other than the opportunistic pathogen, ETBF, to provide extra reassurance about species diversity.
- If some of these species are <DL or have lower than the expected abundance, this can provide extra insight into the extent of the missing microbe picture.
- If Bacteroides thetaiotaomicron is present and more abundant than expected, with some of its fellow Bacteroides missing, this can encourage it to shift fuel source to mucin and drive further GIT imbalances.
Commensal depletion can go on to drive other patterns within a stool test, including:
- Increased abundance of Gram negative (e.g. Fusobacterium nucleatum) and Gram positive bacteria (e.g. Staphylococcus aureus). Indeed, depleted commensal bacteria may often be an upstream cause of Gram negative and -positive overgrowth.
- Reduced mucosal immunity e.g. low sIgA.
- Increased clinical significance of intestinal parasites.
How to Nurture Our Inner Rainforest
- A comprehensive microbiome and host markers private stool test can help us to assess the degree to which compromised diversity and abundance of the commensal gut microbiota. For many clients, this may be the main type of GIT imbalance present. Identifying and addressing these patterns, as guided by Healthcare Provider, can be instrumental in their healing journey.
- Ample consumption of a wide diversity of fibre is the cornerstone of ensuring a health commensal gut microbiome, principally through its ability to support bacterial syntrophy. Research indicates that we need to aim for at least 30 different types of plant each week.(37)
- A good proportion of this daily fibre intake should be prebiotic fibre, the type of fibre which fulfils the ‘prebiotic’ definition of a substrate which selectively supports the growth of commensal bacteria which then confers a health benefit.(38) Key food sources include onion, chicory, plantain, Jerusalem artichoke, and pulses and legumes.
- The prebiotic, galactoligosaccharides (GOS), has the stand-out ability to increase large intestinal colonies of Bifidobacterium since this genus possesses the enzyme β-galactosidase which is needed to process the enzymes in GOS.(39) It can also support Lactobacillus spp.(40) Increasing daily intake of GOS can be a tailored prebiotic intervention when either of these commensals are shown to be depleted and/or when this is suspected due to clinical symptoms which GOS has been shown to improve, such as IBS and atopy.(39,41)
- When no specific commensal is missing but the commensal bacteria generally look depleted, partially hydrolysed guar gum (PHGG) can provide great broad-spectrum prebiotic support with a demonstrated ability to normalise bowel motility and stool consistency.(42,43) Other sources of prebiotic to consider increasing include fucoidan from brown seaweed,(44) colostrum,(45) and polyphenols (e.g. from pomegranate, aronia berry).(46,47) Polyphenol prebiotic support is usually indicated when there is a pattern of mucosal barrier degradation, since those from aronia berry for example can increase Akkermansia colonies.(46)
- Increased intake of probiotics can further improve health outcomes through the functional benefit which they provide as they move through the GIT. The Ecologic® Probiotics blend of carefully selected strains ( bifidum W23, B. lactis W51 and W52, L. acidophilus W37, L. brevis W63, L. casei W56, L. salivarius W24, L. lactis W19 and W58) can improve the integrity of the gut barrier by modulating tight junctions in vitro,(48) with human clinical trials showing systemic health benefits, including for mental health.(49)
- Probiotic supplementation can synergise well with targeted prebiotic support when specific species are depleted, notably Lactobacillus and Bifidobacterium spp., so a client can benefit from the functional benefit of the probiotics as they move through while nurturing the colonies with the prebiotics.
- In severe missing microbe scenarios, increased intake of the ready formed products of beneficial bacteria, so-called ‘post-biotics’, can be helpful to improve health outcomes as quickly as possible, alongside probiotic and prebiotic support.(50) This includes butyrate to support gut barrier integrity, which can be increased through food (e.g. organic, unsalted, grass-fed butter, parmesan) and supplementation.
- Reduce exposure to stressors of the commensal gut microbiota as mentioned previously, especially those which negatively affect specific microbes shown to be depleted, such as a high-fat diet which may deplete Akkermansia according to animal research.(51)
Here at Invivo Healthcare, we often discuss how the decline in ecosystem species diversity on a global scale is mirrored in the decline in species diversity which is now being observed within the human gut microbiota. This falls in line with current thinking about the interconnectedness of every ecosystem on the planet and the current extinction threat to plant and animal communities worldwide.(52,53) We are part of an interconnected ecosystem and only by taking care of all parts of the chain will we significantly improve human health, for now, and in the future. Awareness of this highlights the importance of thinking big when it comes to improving human gut microbiota diversity and asking ourselves, how can I help to nurture the wider ecosystem which I live in too? This can take many forms, such as making a commitment to embracing organic and regenerative agriculture, greener modes of travel, composting at home, or getting involved in litter picking in your local area. After all, we cannot be truly well in an unwell world!